Medical services
Introduction to Hematology
Course Introduction

Blood is the only tissue that flows throughout your body. This red liquid carries oxygen and nutrients to all parts of the body and waste products back to your lungs, kidneys and liver for disposal. It is also an essential part of your immune system, crucial to fluid and temperature balance, a hydraulic fluid for certain functions and a highway for hormonal messages.
This wonderful tissue may be the easiest to transplant (transfuse).
Course Outline
Section One: The Basics
The cell
The Cell
 The cell is the basic microscopic unit of your body. The major cellular structures that we will talk about in this unit are shown in this very simplified drawing.
The cell is the basic microscopic unit of your body. The major cellular structures that we will talk about in this unit are shown in this very simplified drawing.
The nucleus contains the DNA that controls the cell’s function and allows it to respond to its environment. The cytoplasm that surrounds the nucleus contains small structures that make proteins, structures that supply the cell’s energy, molecules that transport energy, chemical messengers, and many other functional elements, as well as storehouses of enzymes and other substances (the cytoplasmic inclusions or granules). The cell membrane controls the flow of substances into and out of the cell and contains molecules called antigens that are specific to the cell and the person.
3D Image: Copyright Bristol Productions
Cell specialization
Cell Specialization
 Mature cells are usually specialized. As cells mature, their shape and contents change so that they can be most efficient at the work that they must do.
Mature cells are usually specialized. As cells mature, their shape and contents change so that they can be most efficient at the work that they must do.
In the blood, all of the white blood cells keep their nuclei so that they can alter their function to meet the challenges of protecting the body from invaders. The red cells, however, lose their nuclei and fill up with the special oxygen-carrying molecule, hemoglobin. They also assume a special shape that is flexible, yet allows rapid transfer of oxygen into and out of the cell.
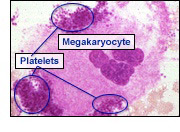 The large cell shown here, the megakaryocyte, stays in the bone marrow after it differentiates from the stem cell. Megakaryocytes are like factories. They manufacture and shed millions of little pieces of themselves into the blood. These pieces of cell, called platelets, contain the substances necessary to help blood clot.
The large cell shown here, the megakaryocyte, stays in the bone marrow after it differentiates from the stem cell. Megakaryocytes are like factories. They manufacture and shed millions of little pieces of themselves into the blood. These pieces of cell, called platelets, contain the substances necessary to help blood clot.
Cell maturation
Cell Maturation
Not all cells are capable of dividing to make new cells. Cells start from a “parent” or stem cell, but then, under instructions from the rest of the body, they begin to specialize and mature. They may alter almost anything and everything about themselves to get ready to do a specific job or set of jobs. They may change shape, their nucleus may be discarded, they may attach to other cells or shed little pieces of themselves. They may make and secrete certain substances or make the substances and store them until they are to be used.
All of the mature blood cells come from one type of precursor, a stem cell.
RBC Photo: Copyright Dennis Kunkel, University of Hawaii
Careers
Careers
Blood is so important to health care that the careers that deal with research of blood: its collection, care, transport, and administration; and its diseases and uses, cover a spectrum of society. There are many many career paths that have to do with blood.

Obviously there are physicians, especially those specializing in hematology, oncology or pathology, but there are many, many others such as physician assistants, nurse clinicians, laboratory specialists, basic research scientists, molecular biologists, epidemiologists, immunologists, statisticians, engineers, research and laboratory technicians, nurses, phlebotomists, chemists… the list goes on and on.
Section Two: What is Blood?
What is blood?
What is Blood?
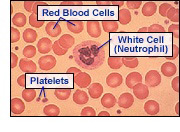
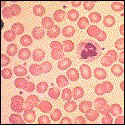
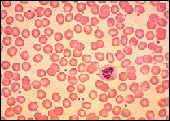
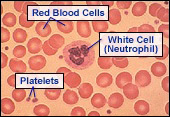
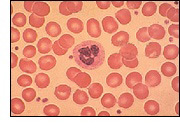 Micorscope View: Although blood appears to be red liquid it is actually composed of a yellowish liquid called plasma and billions of cells. The vast majority of these cells are red cells and these give blood its red color. Besides the red cells, the blood also contains several types of infection-fighting white cells and tiny cell fragments called platelets which are essential for clotting.
Micorscope View: Although blood appears to be red liquid it is actually composed of a yellowish liquid called plasma and billions of cells. The vast majority of these cells are red cells and these give blood its red color. Besides the red cells, the blood also contains several types of infection-fighting white cells and tiny cell fragments called platelets which are essential for clotting.
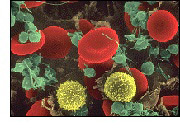 Scanning EM View: These cells have been electronically colored to show up in this photo from a scanning electron microscope (EM). The red cells are shown in red, the white cells in yellow and the platelets in green.
Scanning EM View: These cells have been electronically colored to show up in this photo from a scanning electron microscope (EM). The red cells are shown in red, the white cells in yellow and the platelets in green.
Photo: Copyright Dennis Kunkel, University of Hawaii
How blood cells are made
Blood is Made in the Bone Marrow
All of the cells in the blood, red blood cells, all types of white blood cells, and platelets are made in the bone marrow. This happens primarily in the flat bones in your body such as the skull, the sternum, and the pelvis.
Blood Cell Development
All of the cells differentiate from one group of “master cells” called stem cells. The stem cells can become whatever kind of blood cell the body needs. They come under the influence of factors in their environment to become red cells, white cells, or platelets.
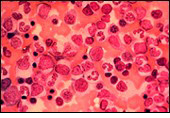
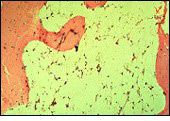
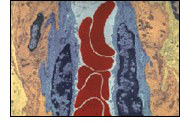
Bone Marrow
This microscopic view of a sample of bone marrow shows mature and immature white cells, the cells that produce platelets and both mature and immature red cells. Notice the variety.
Bone Marrow
Plasma
Plasma
 The plasma is the river in which the blood cells travel. It carries not only the blood cells but also nutrients (sugars, amino acids, fats, salts, minerals, etc.), waste products (CO2, lactic acid, urea, etc.), antibodies, clotting proteins (called clotting factors), chemical messengers such as hormones, and proteins that help maintain the body’s fluid balance.
The plasma is the river in which the blood cells travel. It carries not only the blood cells but also nutrients (sugars, amino acids, fats, salts, minerals, etc.), waste products (CO2, lactic acid, urea, etc.), antibodies, clotting proteins (called clotting factors), chemical messengers such as hormones, and proteins that help maintain the body’s fluid balance.
When you spin blood in a centrifuge, the red cells go to the bottom of the container, and the white cells and platelets to the middle, leaving the yellowish plasma at the top.
Diseases Related to Plasma
 Perhaps the most well-known disease related to plasma is hemophilia. An inherited change in one of the clotting proteins (called factor VIII) leaves it dysfunctional. This single change disrupts the entire sequence of chemical reactions necessary for clotting. As a result, people with hemophilia can suffer severe swelling, bruising and bleeding from simple day to day events that the rest of the population take for granted.
Perhaps the most well-known disease related to plasma is hemophilia. An inherited change in one of the clotting proteins (called factor VIII) leaves it dysfunctional. This single change disrupts the entire sequence of chemical reactions necessary for clotting. As a result, people with hemophilia can suffer severe swelling, bruising and bleeding from simple day to day events that the rest of the population take for granted.
Hemophilia
The child shown above has a severe swelling on the forehead from a bump to the head. This was caused by a failure of his clotting system to stop the bleeding from a bruise. Hemophilia can be controlled with the infusion of factor VIII collected from donated blood or plasma.
Red Blood Cells
 Most of the cells in the blood are red blood cells. These are highly specialized cells that have been “stripped” of everything, including the nucleus, that might get in the way of doing their major job, transporting oxygen.
Most of the cells in the blood are red blood cells. These are highly specialized cells that have been “stripped” of everything, including the nucleus, that might get in the way of doing their major job, transporting oxygen.
Photo: Copyright Dennis Kunkel, University of Hawaii
Hemoglobin
Red blood cells are filled with a special red colored molecule called hemoglobin. It picks up oxygen in areas where oxygen is abundant and releases oxygen in tissues where the oxygen concentration is lowest.
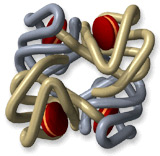
3D Image: Copyright Bristol Productions
Diseases of Red Blood Cells
Diseases of the red blood cells include problems in the development of the cells, infections, destruction in the circulation, and genetic problems. Many start in the bone marrow where red cells differentiate and develop from the stem cells before they enter the circulation.
Normal Red Cell Development
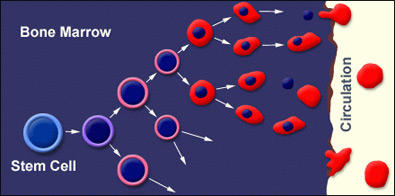
Normally, the bone marrow makes a constant supply of red cells. These cells mature, enter the circulation, do their job for about 120 days, die and are recycled. If more cells are needed (i.e., there is bleeding and loss of red cells, or if a unit of blood is donated) the body easily compensates.
However, there are circumstances in which the body cannot keep up. Too much bleeding, not enough nutrients like iron, diseases that slow down production, increased cell destruction and genetic disorders that affect production or survival are a few of the causes of anemia.
Too Few Cells Made: Developmental Diseases of
Red Blood Cells
Low Production
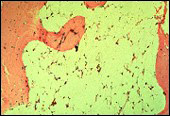
Sometimes the bone marrow cannot keep up with the demand for red blood cells due to destruction of the stem cells themselves. When stem cells are missing, the marrow is an empty place. All of the cell-making activity disappears. This is an extremely dangerous situation which will be fatal if not corrected.
 Aplastic “Empty” Bone Marrow |
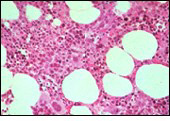 Normal Bone Marrow |
Too Little Hemoglobin: Nutritional Diseases of
Red Blood Cells
Iron is Necessary to Make Hemoglobin
Nutritional diseases of the red blood cells often cause problems in the development of the cells. In cases of iron deficiency there is not enough iron to complete the heme part of hemoglobin.
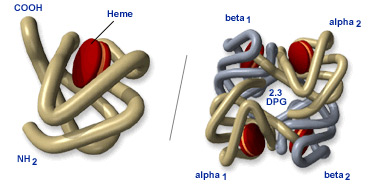
3D Images: Copyright Bristol Productions
Iron Deficiency
The cells on the right were taken from a patient with iron deficiency. The cells arrived in the circulation without enough hemoglobin to carry an adequate amount of oxygen to all parts of the body.
 Normal |
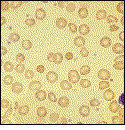 Low Iron |
Flawed Hemoglobin: Genetic Diseases of Red Blood Cells
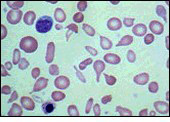
 Click on the image for more information on sickle cell disease. |
|
Hemoglobinopathies
Hemoglobin, the main molecule in the red blood cells, can show a number of genetic differences. Some cause severe problems and some cause no problems whatever.
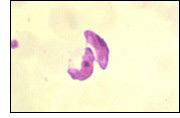
Sickle Cell Anemia
One of the most common genetic alterations causes the hemoglobin to polymerize or form long strands when oxygen to the cell is very low. These long strands stretch the cells into long “sickle” shapes found in sickle cell anemia.
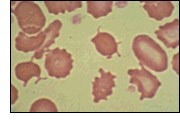
Thalassemias
Other inherited disorders called thalassemias cause an imbalance in the supply of molecular parts (the globin) which make up hemoglobin.
 Beta Thalassemia |
|
Beta Thalassemia
When a thalassemia prevents hemoglobin from forming properly, the blood cells may become misshapen and fragile. Notice that these are all very lightly colored. This condition, called hypochromia, is because they have too little hemoglobin to provide the normal color to the cells.
Fragile Red Blood Cells
Some diseases leave the red blood cells fragile or stiff and inflexible. Cells which break easily and cells that are too stiff to bend and squeeze through the capillaries and the tiny filter-like pores in the spleen are destroyed. If there are too many such cells, the bone marrow can’t keep up and too few red cells stay in the circulation.
Thalassemias
 Beta Thalassemia |
 Alpha Thalassemia |
When a thalassemia prevents hemoglobin from forming properly the blood cells may become misshaped and fragile.
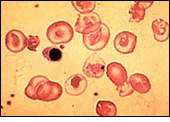
Premature Destruction of Red Cells: Parasites
 Malaria
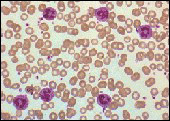
Malaria
Red blood cells can be infected by various bacteria or parasites. In warmer, mosquito-infested areas, the malaria parasite may be passed to humans through the bite of a mosquito. The growth cycle of this parasite can cause massive, life-threatening loss of red cells with fever and anemia.
 Liver Disease
Liver Disease
Red blood cells can be damaged and destroyed when problems occur in the organs such as the kidneys or liver.
Red Blood Cell Flexibility
 Red Blood Cells in Capillary: The special shape and flexibility of the red cell allows it to traverse the narrowest of vessels, the capillaries, to deliver oxygen to all of the cells of the body.
Red Blood Cells in Capillary: The special shape and flexibility of the red cell allows it to traverse the narrowest of vessels, the capillaries, to deliver oxygen to all of the cells of the body.
Photo: Copyright Dennis Kunkel, University of Hawaii
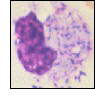
White blood cells
There are five distinctly different kinds of white blood cells, neutrophils, monocytes, lymphocytes, eosinophils and basophils. Some have the ability to change with needs and situations in the body. So, for example, there are different monocytes found in different tissues, and different types of lymphocytes with different roles in fighting infections. These cells can leave the bloodstream, sliding out through the vessel walls and attacking invaders at the site of an infection.
 Neutrophil |
 Monocyte |
 Lymphocyte |
 Eosinophil |
 Basophil |
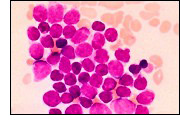
Diseases of White Blood Cells
 As you might suspect from the number of types of white blood cells (also known as leukocytes), and the number of functions, there are many diseases that involve these cells. The term leukemia refers to a great number of these diseases and generally describes cancerous conditions where there are too many leukocytes in the blood.
As you might suspect from the number of types of white blood cells (also known as leukocytes), and the number of functions, there are many diseases that involve these cells. The term leukemia refers to a great number of these diseases and generally describes cancerous conditions where there are too many leukocytes in the blood.
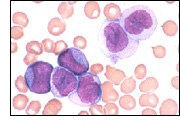
 There are many leukemias. In all of them, one cell line (sometimes lymphocytes, sometimes monocytes, sometimes one of the other cell lines) begins uncontrolled growth. The cells begin to fill the marrow (as shown here) crowding out other cell lines and pouring into the bloodstream.
There are many leukemias. In all of them, one cell line (sometimes lymphocytes, sometimes monocytes, sometimes one of the other cell lines) begins uncontrolled growth. The cells begin to fill the marrow (as shown here) crowding out other cell lines and pouring into the bloodstream.
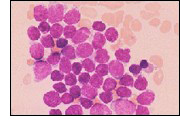
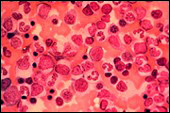
Other, non-cancerous events may trigger higher than normal numbers of white cells. They may be made in response to infection, as shown here on the left. Compare the concentration of neutrophils to the normal smear on the right.
 |
 |
Fighting Infection
 Lymphocytes
Lymphocytes
Each of the white blood cell types has a task in helping the body fight infections. The lymphocytes help create antibodies that attack the invaders and mark them for destruction by the neutrophils, monocytes and macrophages.
 Macrophages
Macrophages
Macrophages (a form of monocyte) engulf invaders and destroy them with powerful enzymes. The macrophage shown here is attacking streptococcus bacteria that cause pneumonia.
Platelets
Platelets are fragments of a much larger cell, the megakaryocyte, that stays in the bone marrow after it differentiates and matures from the stem cell.
 |
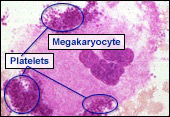 |
The platelets leave the bone marrow and circulate throughout the body. When stimulated by substances from damaged tissue, the platelets release substances necessary to help blood clot. This helps initiate the clotting sequence and protect the integrity of the vasculature.
Diseases of Platelets
When there are too few platelets, a condition known as thrombocytopenia, the blood fails to clot properly. Often many tiny areas of bleeding may be seen under the skin.

Section Three: Blood Banking
Blood banking
 We have known for some time that blood can be transfused to those who need it. The blood must be collected from healthy donors and stored with great care. It is tested for the presence of any infectious diseases, and typed to determine its immune character so that it can be properly matched with a recipient. Once a call comes for a particular type of blood it is swiftly transported to the place of use.
We have known for some time that blood can be transfused to those who need it. The blood must be collected from healthy donors and stored with great care. It is tested for the presence of any infectious diseases, and typed to determine its immune character so that it can be properly matched with a recipient. Once a call comes for a particular type of blood it is swiftly transported to the place of use.
 Modern techniques allow us to separate some of the blood into its parts, such as red cells, platelets, plasma and clotting factors. We can deliver just the parts that the patient may need. In this way, a single donor may help more than one recipient. More recently we have learned to collect only certain portions of the blood such as the plasma, the white cells or the platelets from special donors through a process called apheresis. Finally, we have learned to replace the entire blood-making mechanism within the bone marrow through bone marrow or stem cell transplantation for those with particularly life-threatening diseases.
Modern techniques allow us to separate some of the blood into its parts, such as red cells, platelets, plasma and clotting factors. We can deliver just the parts that the patient may need. In this way, a single donor may help more than one recipient. More recently we have learned to collect only certain portions of the blood such as the plasma, the white cells or the platelets from special donors through a process called apheresis. Finally, we have learned to replace the entire blood-making mechanism within the bone marrow through bone marrow or stem cell transplantation for those with particularly life-threatening diseases.
Blood typing
 In 1901, Karl Landsteiner reported that blood had TYPES. By matching these types one could achieve success in blood transfusion.
In 1901, Karl Landsteiner reported that blood had TYPES. By matching these types one could achieve success in blood transfusion.
The basis of these types are specific proteins called antigens that are found on the surface of red blood cells and antibodies found in the plasma.
There are four basic types:
1. Type A with A antigens on the red cells and anti B antibodies in the plasma
2. Type B with B antigens on the red cells and anti A antibodies in the plasma
3. Type AB with both A and B antigens on the red cells and no type antibodies in the plasma
4. Type O with no type antigens on the red cells and both anti A and anti B antibodies in the plasma
If we take the antibodies from the plasma of a person with type A blood (anti B antibodies) and mix them with the blood (remember…mostly red cells) of a person with type B blood, the antibodies attach themselves to the red cells and cause the red cells to clump together.
These types (and other less striking types) must be properly matched for a blood transfusion to work.
Blood Groups
The various ABO blood groups occur in the average population of the US in the proportions shown here. 45% of the population are type O, 42% type A, 10% type B and 3% type AB. These percentages vary within different ethnic groups. In addition there is another type antigen to be considered. The Rh antigen.
Do You Know Your Blood Type?
Those who have the Rh antigen on their red cells are typed Rh positive while those without it are Rh negative. Thus, when matching blood, we must consider both the ABO system and the Rh types. For example, if you have both the A antigen and the Rh antigen on your red cells, you are A+.
Apheresis
 We must pool platelets from six whole blood donors to provide enough for one transfusion patient.
We must pool platelets from six whole blood donors to provide enough for one transfusion patient.
However, there is a more efficient technique called apheresis that allows us to collect enough platelets from a single donor and then give the donor back all of his or her plasma and red cells. Even then, this is such a small percentage of the donor’s platelets that there is no risk of bleeding problems.
When blood is spun in a centrifuge, it separates into its components with the plasma on top, the white cells and platelets in a thin middle layer, and the red cells on the bottom.
| Blood Passes from Donor to Centrifuge.Plasma and Red Cells Returned to Donor |  |
Platelets Collected | ||
 With the special apheresis centrifuge, the blood can be fed into the system continually. As it spins, the components separate and the platelets are drawn off. The plasma, white cells, and red cells are then recombined and returned to the donor.
With the special apheresis centrifuge, the blood can be fed into the system continually. As it spins, the components separate and the platelets are drawn off. The plasma, white cells, and red cells are then recombined and returned to the donor.
The donor can sit and read, listen to music or watch television while the lifesaving platelets are collected. The body will replace the donated platelets within 72 hours.
Bone marrow transplantation
 The term bone marrow transplant may call up visions of cutting out pieces of bone. However, it is really the transfer of stem cells from a donor to a recipient. Mechanically the technique has more in common with transfusion than with organ transplantation.
The term bone marrow transplant may call up visions of cutting out pieces of bone. However, it is really the transfer of stem cells from a donor to a recipient. Mechanically the technique has more in common with transfusion than with organ transplantation.
One of the most common reasons for a bone marrow transplant is that the patient has a leukemia that will not respond to chemotherapy. In these patients, any treatment that removes all of the tumor cells from the marrow also kills the stem cells thus leaving the patient with no ability to make new blood cells
  |
Finding a donor for bone marrow transplantation can be very difficult. The donor must match the patient not only in ABO type as in transfusion, but in hundreds of type characteristics. Remember, when we replace stem cells we are providing a whole new blood system complete with white blood cells that will try to fight anything foreign.
Once a donor is found, the patient’s bone marrow and all of the tumor cells are killed leaving an empty marrow.
With the donor under anesthesia, marrow is aspirated (drawn) out of the iliac crest of the pelvis (hip bones). This is only a small portion of the donor’s marrow and is soon replaced.
This marrow is filtered and treated to remove bits of bone and other unwanted cells and debris, is transferred to a blood bag, and is infused into the patient’s blood, just like a transfusion.
 Normal Bone Marrow |
The donor’s stem cells find their way into the patient’s empty marrow and begin to produce all of the blood cell types.
Another technique, stem cell transplantation, is providing an alternative for some patients. New technology now allows collection of stem cells by apheresis, rather than the surgical procedure of bone marrow collection.
At the end of a successful bone marrow or stem cell transplantation, the patient’s marrow is repopulated with growing cells that are constantly being added to the patient’s bloodstream….the normal healthy cycle of cell development, specialization, aging and replacement.

